32 YR OLD MALE WITH INVOLUNTARY MOVEMENTS

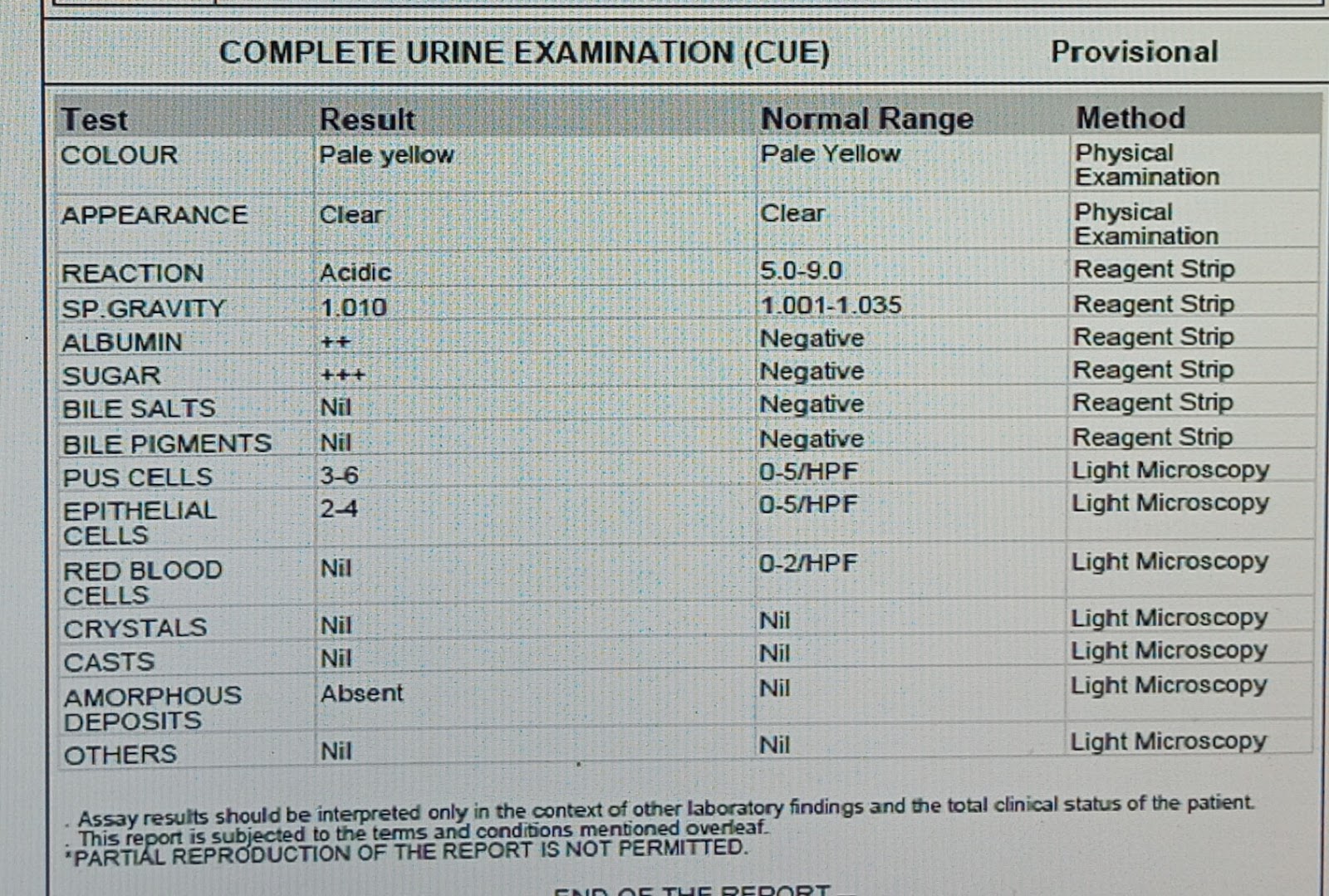
202410956 M Nagu CASE HISTORY AND CLINICAL FINDINGS PATIENT WAS BROUGHT TO CASUALITY WITH H/O INVOLUNTARY MOVEMENTS MULTIPLE TIMES SINCE 2 DAYS HOPI PATIENT WAS APPRENTLY ASYMPTOMATIC 2 DAYS AGO THEN HE DEVELOPED ONE EPISODE OF SEIZURE LIKE ACTIVITY AT 11 PM ON 6/3/24 .ONE EPISODE AT 9PM ON 7/3/24,4 EPISODES WITH 5 MINUTES INTERVAL AT 12 AM ON 7/3/24 EACH EPISODE LASTING FOR 5- 10 MINUTES WITH INVOLUNTARY MOVEMENTS OF ALL FOUR LIMBS.FROATHING FROM MOUTH PRESENT,UPROLLING OF EYEBALLS PRESENT TONGUE BITE ABSENT INVOLUNTARY MICTURITION,DEFEACATION ABSENT H/O VOMITING FOR 2 DAYS ,3 EPISODES PER DAY,FOOD AS CONTENT,NON BILIOUS NO H/O HEAD TRAUMA,FEVER,LOOSE STOOLS PAST HISTORY; K/C/O DM SINCE 6 YEARS ON REGULAR MEDICATION ON TAB.GLICLAZIDE 60MG PO/OD N/K/C/O HTN,EPILEPSY,CAD,CVA,ASTHAMA,THYROID GENERAL EXAMINATION PT IS C/C/C PR - 104BPM BP - 180 / 100 MMHG RR - 20 CPM TEMP - 98 F GRBS - 312 MG /DL CVS - S1 S2 PRESENT RS - BAE PRESENT , NVBS P/A - SOFT , NON TENDER PSYCHIATRY REFERRAL ON 8/...