59 K. Rithika Vasantha
Greetings to one and all who are currently reading my blog. This is Rithika, a third semester medical student.
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
Note : This blog had been done under the guidance of Dr. Jancy ( Intern)and Dr. Roshini. ( Intern).
A 60 year old female with CKD
CHIEF COMPLAINTS :
• Cough since 3 months
• Loss of appetite and nausea since 10 days
• Generalized weakness and unable to get up from bed since 3 days
• Decreased urine output since 3 days
• Constipation since 3 days
• Altered sensorium since 2 days
• SOB - grade III since 1 day
HISTORY OF PRESENT ILLNESS:
• Patient is a daily wage labourer . She stopped working 1 yr ago when her husband passed away . And due to generalised weakness since then, she is staying at home. But, does her regular activities at home.
• Our patient was apparently asymptomatic 3 months back.
• Then developed cough, which was productive and non-relieving with medication and SOB grade IV
HISTORY OF PAST ILLNESS:
• 6 years ago, she had history of fever and generalized edema , facial puffiness , loss of appetite for which she visited a local hospital , where they told her she has a renal failure and was on medications. No decreased urine output at that point of time.
• Her edema subsided after using medications . She stopped using medications after few days as she was feeling well.
• She has history of dry cough and SOB since 6 years.She self diagnosed herself with tuberculosis and used her husband's TB medications on SOS basis.
• Her husband had history of chronic cough - ? Pulmonary kochs and expired last year at home.
• After her husband expired, Pt. began smoking again.
• 8 months ago, she complained of facial puffiness , but no pedal edema . Low grade fever, burning micturition.
• She went to local hospital and edema subsided with medications.
• Since 3 months pt complained of intermittent low grade fever , loss of appetite.
• Cough since 3 months, associated with scanty sputum , white colour. Generalized weakness and body pains.
• No history of weight loss as per attenders.
• Pt went to local hospital where she was told that she had pneumonia and used medications. But her symptoms didn't subside.
• Attenders also gave history that she tested for tuberculosis , but it was a negative. ( Previous reports / prescriptions not available)
• She was using intermittently dytor plus tablets.
• Since 3 days, she has generalized weakness, Decreased urine output and constipation.
• Altered sensorium, irritable and irrelevant talk since 2 days.
• SOB - grade III since 1 day
TREATMENT HISTORY:
• She has no treatment history of DM, HTN, CAD, asthma, TB, Antibiotics, hormones, chemo radiation, blood transfusions and surgeries.
PERSONAL HISTORY:
• Pt is married and has 2 children , full term, normal vaginal delivery at home.
• Her appetite is normal and follows a mixed diet.
• Her bowels are regular and micturition is normal.
• She has few known allergies.
• She has no Comorbidities and has history of NSAID abuse over the past 5-6 years which were used for generalized body aches.
• She is a chronic chutta smoker since 30 yrs, ( 8-10 chuttas per day initially, Since 3 yrs, reduced it to 2-3 chuttas /day)
• She is also, occasionally alcoholic.
FAMILY HISTORY:
• She has no family history of DM, HTN, TB, asthma, strokes, heart diseases, cancers .
GENERAL EXAMINATION:
• Pallor - Yes
• Cyanosis - no
• Lymphadenopathy - no
• Malnutrition - no
• Clubbing of fingers/toes- no
• Oedema of feet - no
• Swelling noted in supraclavicular region, but soft in consistency and mobile ( ? Lipoma / ? Virchows node)
VITALS :
• Temperature - afebrile
• BP - 110 mmHg
• RR - 22 cycles/min
• PR - 117 bpm
• SPO2 - 99%
• GRBS - 120mg%
• Urine output - 30ml ( from 6-7 hrs)
SYSTEMIC EXAMINATION:
A. CARDIOVASCULAR SYSTEM
• S1, S2 are heard
B. RESPIRATORY SYSTEM
• Dyspnoea present
• No wheeze
• Position of trachea - central
• Breath sounds - vesicular
C. ABDOMEN
• Scaphoid shape
• No tenderness, palpable mass, free fluid, hernial orifices, bruits
• Liver and spleen are not palpable
• Bowel sounds - present
D. CENTRAL NERVOUS SYSTEM
• Pt is conscious , with altered sensorium, not oriented to time, place, person.
• Speech normal
• No signs of meningeal irritation
CEREBRAL SIGNS :
• No finger nose coordination and no knee heel coordination.
PROVISIONAL DIAGNOSIS :
CHRONIC RENAL FAILURE WITH UREMIC ENCEPHALOPATHY
? MILIARY TUBERCULOSIS
? ANEMIA OF CHRONIC DISEASE
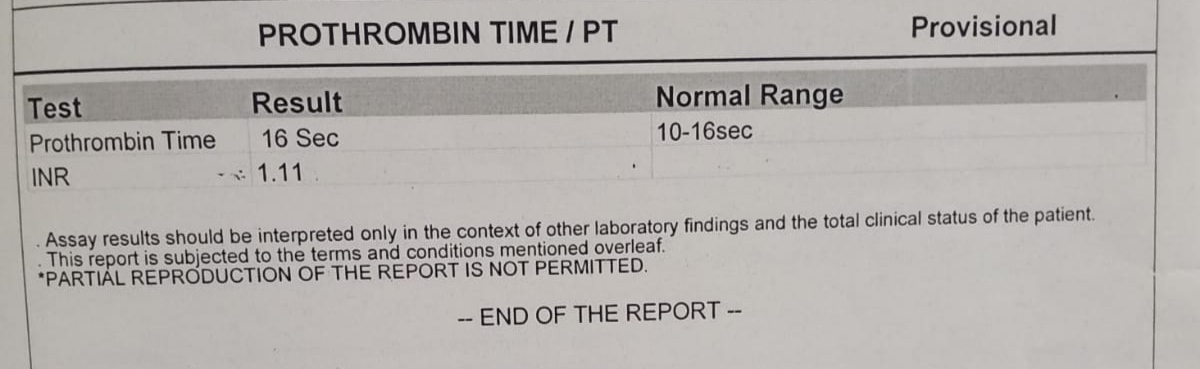
INVESTIGATIONS :
ON DAY 1 ( 16.8.21)
Ultrasound report:
ECG :
DAY 2 ( 17.8.21)
DAY 3 ( 18.8.21)
DAY 4 ( 19.8.21)
Fever chart
TREATMENT :
DAY 1 ( ON 16.8.21)
• Inj. NaHCO3 100mEq IV/STAT
• Inj. PIPTAZ 4.5 mg IV / STAT to Inj. PIPTAZ 2.5 mg IV /TID
• Inj. PAN 40 mg IV / OD
• Inj. ZOFER 4mg IV / SOS
• Tab. NODOSIS 500mg IV/ TID
• Tab. SHELCAL PO / OD
• Tab. OROFER XT PO/ BD
• Inj. ERYTHROPOIETIN 4000 IU / weekly twice
• Strict I/O monitoring
• BP charting 2nd hourly
• GRBS charting 6th hourly
DAY 2 ( 17.8.21 )
• IVF 10 NS@ 75ml/hr ( slow IV)
• Inj. Piptaz 2.25 g
• Inj. PAN 40 mg IV / OD
• Inj. ZOFER 4mg IV / SOS
• Tab. NODOSIS 500mg IV/ TID
• Tab. SHELCAL PO / OD
• Tab. OROFER XT PO/ BD
• Inj. ERYTHROPOIETIN 4000 IU / weekly twice
• Strict I/O monitoring
• GRBS charting 6th hourly
• BP/PR charting 4th hourly
• Inj. Kel 2 Amp. in 500 ml NS IV over 8 hrs
DAY 4 ( 19.8.21)
• IVF - 10 RL - @ 75ml / hr
• Inj. Piptaz 2.25 g
• Inj. PAN 40 mg IV / OD
• Inj. ZOFER 4mg IV / SOS
• Tab. NODOSIS 500mg IV/ TID
• Tab. SHELCAL PO / OD
• Tab. OROFER XT PO/ BD
• Inj. ERYTHROPOIETIN 4000 IU / weekly twice
• Inj. LASIX 20 mg IV/BD
• Tab. B complex PO/OD
• Monitor vitals 4th hourly
• Strict I/O charting
• GRBS charting 6th hourly

































Comments
Post a Comment